Health & Social Development
Mission
In the spirit and intent of our inherent and Treaty Right to Health and in partnership with our member First Nations, Prince Albert Grand Council Health and Social Development supports the delivery of holistic community health and wellness programs.
The Prince Albert Grand Council’s Department of Health and Social Development provides health and social programming and services to our 12 member First Nations. Our department continues to display excellence and innovation through the implementation of the latest in technology and best practices in health care.
Our Treaties serve as a foundation for our health care programs and services at PAGC, and, even though the current health environment has shifted from an exclusive federal Treaty-based premise to a collaborative inter-jurisdictional approach, we continue to promote and protect our Treaty rights when building partnerships with external health and social agencies. An example of our collaboration with our communities is evidenced through regular engagement, participation, and feedback from the PAGC’s Health Directors Working Group, Health Commission Chiefs, and Women’s Commission.
As we plan for the future, we are considering options to improve our health system. One path could lead to an engagement with the Prince Albert Parkland Health Region, related to their hospital renewal plans. The other path may lead to the development of an independent hospital, which we believe has strong potential of becoming a reality with the support of the community, our leadership and joint partners. We are also working on plans to establish a First Nations wholesale prescription drug distribution company. While these projects are a work in progress, we will continue to retain service agreements with health professionals, pertaining to vision care, dental care, physician services and all manners of professional medical services to “occupy the field.”
We pride ourselves on providing the best in health care, and one vital component in ensuring we achieve our goals is through the recruitment of staff who understand the health status of our First Nations communities and have the desire to make a difference.
PAGC’s Department of Health and Social Development provides programs and services in Public Health, Home and Community Care, Primary Care (Hatchet Lake Denesuline Nation), Diabetes Education and Support, Tobacco Control, Dental Therapy, a Medical Reprocessing Facility, Maternal Child Health, Headstart and Daycare, Environmental Health, Indian Residential Schools (IRS) Resolution Support Work, First AID/CPR, Health Facilities and Emergency Preparedness Planning.
Services the Holistic Wellness Centre include: Responsible Gambling Program, Integrated Wellness Coordinators-NNADAP, Sakwatamo Lodge, Embrace Life-Youth Action Councils, Men and Women’s “Honouring Our Traditions Program,” Edu-Therapy Solutions, local Mental Wellness teams, and training in Crisis Intervention Stress Management (CISM), Mental Health First Aid, Applied Suicide Intervention Skills Training (ASIST), safeTALK, grief resolution and trauma training.
Aboriginal Diabetes Initiative
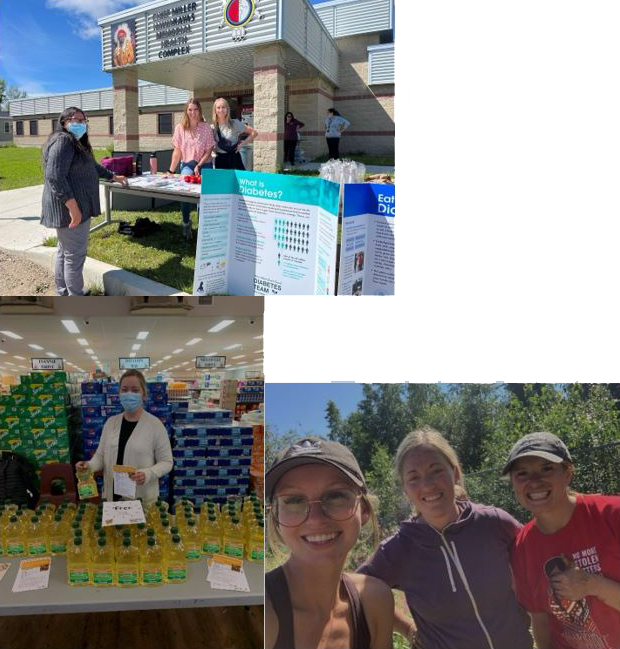
The Aboriginal Diabetes Initiative (ADI) consists of two full-time Registered Dietitians, one part-time Registered Dietitian, and one Diabetes Nurse. Our aim is to improve the overall health and well-being of community members, with and without diabetes, by building capacity within the community and to support health promotion, diabetes prevention, and self-management of diabetes. We provide individual and group education on topics such as healthy eating, food skills, and chronic disease prevention and management. The program is delivered to the communities of Wahpeton Dakota Nation, Little Red River Reserve, Montreal Lake Cree Nation, Shoal Lake Cree Nation, Red Earth Cree Nation, Cumberland House Cree Nation, and Hatchet Lake Denesuline Nation.
Food Security initiatives have been undertaken in several PAGC communities. Projects have included community and cold frame gardens, cooking classes and grocery store tours. We also collaborate with the Head Start On-Reserve and Daycare Programs to implement new menu planning guidelines, and, in conjunction with Maternal Child Health, we offer healthy living programs to families.
The ADI team provides presentations and displays at PAGC initiatives, such as conferences, assemblies, health fairs, Treaty Days, and community events. We also participate with health promotion committees to enhance the work of the ADI team in sharing the knowledge, resources, and partnerships with the communities. We routinely collaborate with other health agencies to provide an interdisciplinary and intersectoral approach to client care and mentor students from the University of Saskatchewan Nutrition and Dietetics Program.
Canada Prenatal Nutrition Program
Canada Prenatal Nutrition Program (CPNP) aims to improve the health of pregnant women, new mothers, and their babies by supporting healthy pregnancies and promoting and supporting breastfeeding. Prince Albert Grand Council (PAGC) Public Health Nurses facilitate CPNP in partnership with the Maternal Child Health program in six communities: Wahpeton Dakota Nation, Little Red River Reserve, Hatchet Lake Dene Nation, Cumberland House Cree Nation, Red Earth Cree Nation and Shoal Lake Cree Nation. CPNP is supported by PAGC’s Registered Dietitian team who are based out of Prince Albert.
Examples of community programming that support the program include nutrition counseling appointments with a Registered Dietitian, cooking classes, food voucher programs, baby food making workshops, and breastfeeding education and support.
Nutrition North Canada
The purpose of Nutrition North Canada (NNC) is to support access to fresh and healthy foods in remote communities. Prince Albert Grand Council receives funding for the nutrition education component of NNC for the community of Hatchet Lake Dene Nation. Examples of community programming include freezer meal classes, Food of the Month displays at the local grocery store, gardening initiatives, and support for community caribou hunts.
Daycare & Headstart
Early Learning and Child Care Programs for Prince Albert Grand Council are delivered to 11 communities. These programs help create a foundation for life-long learning, school readiness and promote health and well-being. Aboriginal Head Start has a parent component, along with the same six components guiding daycare: Culture and Language, Education, Health Promotion, Nutrition, Social support, and Parent Involvement. Daycare programming is provided in a multi-age group setting.
Dental Therapy
The PAGC Dental Therapy program focuses on oral health and disease prevention, patient education, and overall health. Recognizing oral health and holistic health are linked, we strive to reach out and treat as many patients as possible. The program fills a vital role in the community as it can be the first line of defense in maintaining good health. The priority of the program continues to be focused on providing school aged children with optimal dental treatment and facilitating prevention programs for all community members. Dental Services for the adult population in PAGC communities remains a priority.
The PAGC Dental Therapy program also administers the Children’s Oral Health Initiative (COHI) in our communities. COHI is a community-based service that focuses on preventing dental disease in children from an early age. The COHI program targets children aged 0-7, their parents and caregivers and pregnant women. COHI services include annual screening, fluoride varnish applications, silver diamine fluoride, sealants and temporary fillings and oral health education.
All Dental Therapy staff continue to meet licensing requirements by attending CPR refreshers annually, training for new products and equipment and participating in continuing education sessions. The dental team in Hatchet Lake have recently been trained to safely provide nitrous oxide sedation to patients who are apprehensive or fearful of dental treatment. We continue to strive to have a strong knowledge base to meet the new challenges faced in dentistry.
PAGC is currently under contract with the University of Saskatchewan to provide comprehensive oral health services in the eastern communities. PAGC has also contracted a private dentist to provide these services in the community of Hatchet Lake.
Our dental team is comprised of Dental Therapists, Dental Aides and visiting Dentists. The dental team works together to give all community members the highest standard in patient care. They continue to identify needs of their communities and will educate and promote and stress the importance of receiving dental care from the earliest age possible onto one’s adult life, through well baby clinic, school promotion, prenatal and classroom presentations, and regular dental checkups.
Dental Therapists provide diagnostic, restorative, and preventative services to the children and to adult patients on an emergency basis. The visiting dentists travel to the communities to provide dental services to the adult population and provide dental treatment beyond the scope of the Dental Therapist. Dental Aides provide support services and ensure the continuation of the COHI program. With these combined efforts, all dental services within the PAGC communities will continue to progress.
Jordan’s Principle
Jordan’s Principle ensures all First Nations children living in Canada can access the products, services, and supports they need, when they need them.
Jordan River Anderson was a young boy from Norway House Cree Nation in Manitoba who was born in 1999 with multiple disabilities. He lived over two years in a hospital because federal and provincial governments could not agree on who would pay for his at-home care. The reason for this is that federal and provincial/territorial governments cannot agree on which government should pay for services to First Nations children on reserves so they typically do not provide the service until they can sort out the payment issue.
Unfortunately, Jordan died at the age of 5 before he could experience living in a loving home. Jordan’s death ignited a movement to uphold human rights for all First Nations children through the creation of the child-first principle called “Jordan’s Principle.”
If your child/ren, aged 0-18 and has a disability, or a social, education or health need that is not being met, they may be eligible to receive supports.
HOW TO APPLY
Required Documentation
Please collect the following documentation which are required in order to apply for supports.
Letter of Hardship (Required)
This is letter from yourself, stating your situation and your child’s specific needs.
Letter of Recommendation (Required)
This is a letter supplied to you by a health, social or education professional in your child/ren’s direct circle of care (Teacher/Principle, Guidance Counsellor, Nurse Practitioner/Doctor). The letter is the basis for an approval and should recommend the child’s needs/supports/services, including what the recommended frequency/duration is. The letter should be signed, dated and if applicable, on a letterhead.
Jordan’s Principle Application (Required)
Please fill out the application with as much information as you can. You only need to include one child’s name in the application, but please mention all the children you are applying for, in your recommendation and hardship letters.
You can download the application by clicking the link below.
Quote (If applicable)
In some instances of approval, you may need to provide a quote or a service provider to match the specific needs of the child. If your child has specific needs or services, please include this with your application.
Submit Your Application
Please include the following information in your email when submitting your application. Applications are processed in the order they are received and a coordinator will contact you directly once they get to your application in queue.
Your First Name, Last Name and Phone Number
Letter of Hardship
Letter of Recommendation
Complete Application Form
Quote (if applicable)
Email to: jpservice@pagc.net
We encourage you to include all your documents into one email when submitting your application. This will ensure there is not a high number of emails to sift through, and to avoid lost documents.
When faxing your documents, please include your first and last name in the subject line. This will ensure we can search for your documents if needed.
Important note:
Our office is experiencing a backlog of applications from families that are in need and wait times may be extended. We are working as hard and diligently as possible to get your child the supports they need. A coordinator will contact you directly as soon as they begin processing your application.
Maternal Child Health
The Maternal Child Health and Fetal Alcohol Spectrum Disorder programs are designed to deliver culturally safe programs that acknowledge and respect diversity in each community. All aspects of the Maternal Child Health program are voluntary, strength-based, and culturally safe.
Programming is provided to enhance parenting skills; to educate parents in early childhood development; to promote healthy pregnancies; to prevent Fetal Alcohol Spectrum Disorder; to implement cultural teachings for parents and the community; to engage fathers, as they are important for their children’s over all development; to support a referral process by utilizing the Nipissing District Developmental Screen; and to collaborate with other programs in the community such as the Public Health Nurses, CPNP.
It is important as parents to learn traditional teachings; to learn childrearing practices of long ago; to learn ceremonies for our children relevant to each community; to retain and implement First Nation languages which contributes to our children’s sense of identity as Indigenous people. The home visitors invite Elders and Knowledge Keepers to share their wisdom and knowledge with families.
The home visitors resumed indoor visits with families; the home visitors spend a percentage of their time researching topics related to early childhood development; early brain development and providing home visiting services. In addition, they plan and prepare for their home visits based on the supports identified by the parents. The home visitors offer cultural teachings in collaboration with the Elders and Knowledge Keepers.
The home visitors provided parents with family packages, which includes materials and books. These activities promote parent and child interaction, early literacy, bonding and attachment and family wellness. The home visitors encourage families to implement culture and traditions and encourage parents to teach their children their traditional language.
The parents receive booklets such as Parent’s Are the First Teachers, Family Connections, Fatherhood is Forever, and Growing Up Healthy, which are published by N.C.C.A.H.
Nursing
PAGC’s Nursing Services provide first-level nursing services in Public Health, Home & Community Care, and Primary Care to six PAGC First Nations communities, including Shoal Lake Cree Nation, Red Earth Cree Nation, Hatchet Lake Denesuline, Little Red River Reserve, Wahpeton Dakota Nation and Cumberland House Cree Nation. Support at the secondary level is also provided Sturgeon Lake Cree Nation, James Smith Cree Nation, and Montreal Lake Cree Nation. Comprehensive nursing services are provided through an integrated, holistic Population Health and Primary Health Care models. These models empower and promote wellness and independency amongst individuals, families and communities.
PAGC Nursing Services are responsible for the following functions:
Nursing administration, including management/supervision of nursing and diabetes initiative personnel, obtaining supplies and equipment, and capital resources;
- Recruitment and retention of Registered Nurses and Licensed Practical Nurses for PAGC communities;
- Program development and implementation that reflects current Standards of Practice;
- Program monitoring and evaluation to ensure high quality nursing service delivery;
- PAGC representation on NITHA Working Groups, FNIH and FSIN Working Groups;
- Liaising with other health agencies, including three regional health authorities; and,
- Collaboration with other PAGC service providers in ensuring an interdisciplinary team approach.
Public Health
Public Health (Community Health) focuses on these essential nursing functions: health promotion, disease and injury prevention, health protection, health surveillance, population health assessment, and, emergency preparedness and response.
Public Health nurses complete these functions through programming in immunization, communicable disease, maternal child health, school health and the chronic disease program.
Communicable diseases, including immunization, are mandatory programs. This year, our Influenza Program included an “immunize or mask” policy similar to the province and other jurisdictions across the country. This program requires that any staff having contact with clients must either receive the influenza vaccine or wear a mask during client care from October to April. Most of our communities were successful in implementing this program, resulting in better health for our communities.
PAGC also had a successful Community Influenza Program. As we work to encourage more individuals to be immunized, this year most communities have been immunized at a similar rate as previous years.
One of the goals of our immunization program is to achieve rates over 95%. Once this rate is achieved, we will have herd immunity, which means that enough people have been immunized to prevent the bacteria or virus from being able to spread.
Home & Community Care
The Home & Community Care Program is based on five essential elements, including assessment (case management, linkages, referrals, medical supplies and equipment), nursing services (education, medication monitoring and health assessment), personal care (by Certified Home Health Aides), home management (house cleaning, water delivery, reassurance visits), and in-home respite. Program management, supervision, and data collection are also included.
The goal of the Home & Community Care is to assist clients to maintain optimum health and remain living independently in their communities by assisting clients and family members to meet the client-assessed care needs. The program supports and improves the care provided by family and community but should not replace it.
Primary Care
Services for primary care are provided in the community of Hatchet Lake Denesuline Nation. Generally, these services are provided by Registered Nurses with advanced clinical skills under the Transfer of Medical Function. These services include 24-hour medical emergency care and advanced clinical nursing services.
The policies and procedures for Transfer of Medical Function will soon be replaced by Clinical Decision Tools, developed by various health professionals, including the Saskatchewan Registered Nurses Association and physicians. The implementation of clinical decision tools will begin in December 1, 2016. Registered Nurses currently working in this expanded role have also been taking extra courses to meet the competencies required by the Saskatchewan Registered Nurses Association in order to obtain the Advanced Authorized Practice in December 1, 2016.
PAGC’s Registered Nurses with advanced clinical skills dedicate their services to the community of Hatchet Lake Denesuline Nation.
Home & Community Care
The goal of the Home & Community Care Program is to assist families in helping the client in obtaining and maintaining optimum health and to remain living independently in their home and community, as long as it is safe and adequate support is available. It does not replace the responsibilities of the family. To achieve this goal, the program is based on nine essential elements.
Program management and supervision includes scheduling of services, orientation, obtaining office and medical supplies, and supervision of Home Health Aides (HHA). Nursing services include health education, medication monitoring and administration, dressing changes, foot care, health assessments, and monitoring of the client’s health condition, client advocacy. Home support includes personal care by a certified HHA and home maintenance. Finally, data collection includes information collection and data input into the electronic service delivery reporting template (e-SDRT).
The program receives a small amount of funding for Palliative Care. This is used to obtain palliative equipment and supplies for all communities as well as provide palliative on call services on weekends in one community.
PAGC Home Care Nurses are required to obtain training in Foot Care, Wound Care, Case Management and Diabetes’s Education. Staff also have an opportunity to participated in other professional development.
New to the Home and Community Care Program is a Diabetes Nurse Educator, who works closely with the Aboriginal Diabetes Initiative (ADI) Team.
Nurse Navigators
The Nurse Navigator position is a joint venture between PAGC and Saskatchewan Health Authority. The positions are filled by Registered Nurses employed by PAGC. The office is situated at the Victoria hospital with the role being managed by both respective agencies. The initial Nurse Navigator’s main role is to connect with patients and families in the Obstetrics and Pediatric unit at the Victoria hospital. However, the Nurse Navigator is also utilized in other areas of the tower at the Victoria hospital. These additional interactions are only available when requested and resources permit.
The Nurse Navigator role in the Victoria Hospital has made an impact that benefits both staff and the patients they serve.
The Nurse Navigator’s role promotes culture appropriate and safe care for Indigenous people who are seeking service at the Victoria hospital. Supporting a patient’s journey that promotes cultural sensitivity during their hospital stay is essential and assists in an all-around good experience. The patient’s transition to hospital care can be stressful and sometimes difficult, but with the assistance of the Nurse Navigator it can hopefully be put to ease.
The Nurse Navigator is in place to support and enhance existing services in the Victoria Hospital by educating, advocating and being a liaison for patients, families, and staff. The patients benefit through teachings, referrals, and emotional support during their stay at the hospital. For example, medical instructions are explained, as well as the translation of medical terminology, explanation of tests or procedures, informed consent and to ensure care plans are understood. The result is the patient having a positive experience and a greater knowledge/understanding while in hospital, which would continue in the transition back to their home communities.
Another role for the Nurse Navigator is finding Indigenous resources for hospital personnel (i.e. finding an elder or developing a protocol for elder consultations), as well as community programming. Having this bridge of information between patient, care givers and hospital generates the holistic patient care. This promotes reconciliation and understanding of our patients in healthcare, which will lead to treating all with kindness and respect.
Resolution Health Support Services
The Resolution Health Support Services provides information and services to former Indian Residential School (IRS) students/Sixties Scoop/Indigenous Day School (IDA), Missing and Murdered Indigenous Women and Girls (MMIWG) survivors and their families which is part of the Indian Residential School Settlement Agreement (2008). The RHSW program recognizes Intergenerational effects and impacts which will continue to serve clients, individuals who are directly and indirectly affected and impacted by Indian Residential Schools, Sixties Scoop and the Federal Indian Day School Agreements and process.
The RHSWs continue to provide emotional/mental/spiritual support when requested and during Cultural/Elder gatherings, training or information sessions by Health Canada or communities. We work with the Gowlings Law firm before, during, and after their information sessions regarding Day School. We also provide interpreting services in Cree and Dene to the survivors so there is a better understanding of the day school class action process. We also assist when requested to be in care homes, hospitals, home or in the penal institutions.
The Elder continues to assist claimants by providing prayers and smudging. The Elder’s role is vital as many claimants feel safe when an elder is present. The Elder is also available to survivors to make an appointment for one-to-one traditional counseling and also if they request to participate in a traditional event or ceremony.
Since the deadlines of the Common Experience Payment and the Individual Assessment Process has come and gone, the RHSW’s roles have shifted into an educational and healing component. The RHSWs can now facilitate the Kairos Blanket, Grief/Loss, medicine wheel teachings, cultural gathering, land-based teachings, sacred ceremonies, and all training for RHSW’s in the province or out of province. The RHSWs go into schools and communities to speak on the history of the Indian Residential Schools, truth & reconciliation, medicine wheel teachings, grief/loss, cultural gatherings, and traditional ceremonies or land-based teachings. and work towards healing together as a whole. All the training the RHSW’s facilitate are interactive learning opportunities to support all survivors in their individual healing journeys.
For each training is introduced by IRS history and the shaping of the Settlers and Indigenous Peoples relationship. The mandate is to focus on the truth of the past, learn about the present relationship with the government of Canada and Indigenous people as well as to learn the significant aspects of the healing modalities of traditional spiritual ceremonies, methodologies and epistemologies as directed by traditional knowledge keepers.
In addition, cultural gatherings, land-based gatherings, sacred ceremonies, Round Dances, training, information sessions, and support at other gatherings, such as land based, cultural events, and Treaties Days has occurred.
Telehealth
Telehealth is live interactive video conferencing that remotely connects a healthcare provider with a patient. Video conferencing can include desktops, laptops, and mobile devices.
Video conferencing connections are made possible with Community Net (CNET), a private network, that is accessed by authorized users only.
To date, Telehealth Saskatchewan operates from more than 440 sites in 147 communities across the province (https://www.ehealthsask.ca/services/telehealth).
Prince Albert Grand Council Health & Social Development (PAGC H&SD) Telehealth Program has 11 telehealth sites. Nine sites each have one telehealth system. Red Earth and James Smith each have two telehealth systems. A total of 13 telehealth systems.
Nine of the telehealth sites are operational and have trained health staff to operate the telehealth systems. Sakwatamo Lodge telehealth system is offline due to their move to Wahpeton. Cumberland House is temporarily offline for equipment maintenance.
Little Red telehealth site clinical, administrative, and education sessions are scheduled by Roderick Sanderson, Lac La Ronge Telehealth Coordinator.
Video conferencing training will differ for each health staff. Those that are the main and backup telehealth supports are trained with Train the Trainer model. Train the Trainer model is also for any health staff that would like the complete telehealth system training. Introductory training is also provided which involves readying the system for audio/visual, remote-control functions, and how to reset the codec and UPS.
Environmental Public Health
Environmental Public Health Services encompassing the nine program areas were provided to all communities and urban facilities during this reporting period. A team of four Environmental Public Health Officers, a Supervisor and an Administrative Assistant were directly responsible for maintaining the program and service delivery in accordance with Indigenous Services Canada (ISC) requirement. The mandatory programs of Water Quality, Food Hygiene, Housing and Communicable Disease investigation, as well as requests by Chiefs, Health Directors, Home Care Nurses, Community Health Representatives and residents received 100% coverage.
